On Christmas eve, I had a colonoscopy and endoscopy. How’s that for a Christmas gift?
My doctors and I are investigating my otherwise asymptomatic iron deficiency that we found in August. We still haven’t figured it out, but meanwhile, I’ve got to tell you about the procedure, its prep, and the anesthesia.
Prep
I remember distinctly that when I was booked for the last slot on 12/24, I marked all day 12/23 on my calendar as busy too. Why?
See, for gastroenterologists to get in and look around at your colon, your colon needs to be empty. The camera can see through a bit of “clear liquid” like water, but nothing more. Now, if you think about it, that’s a really unnatural state of things! If life has gone well and you haven’t starved or gotten cholera or something, your colon has never been empty in your life. You were even born with a bit of poo: meconium, a tarry green odorless substance, and since then, it’s just been a continuous cycle of more-in-before-all-out. Yup.
Fortunately, science! Colonoscopy prep is a whole ordeal with many separate steps to make sure nothing brown and/or solid is stuck in the tube that is your GI tract.
Different foods adhere to the intestinal walls differently, so for 3 days, I ate a low-residue low-fiber diet. For me, that meant no fruit and no vegetables, so I ate more rice and white bread instead of veggies and snacked on cookies instead of apples. Super healthy.
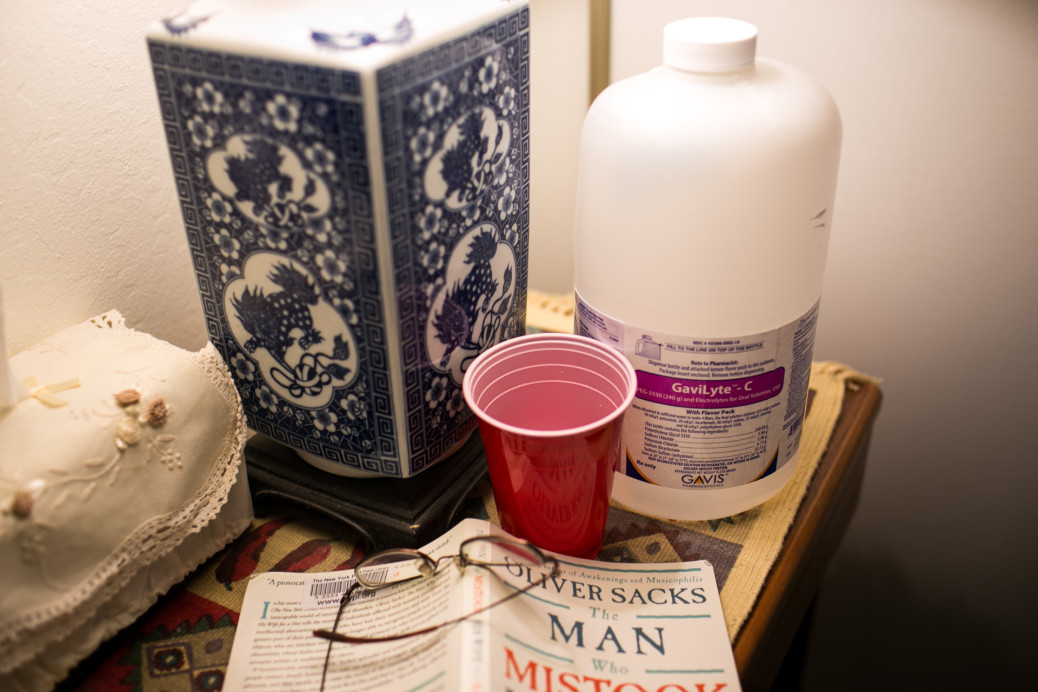
Our bowels have a 12-18 hour turnaround time for most substances, so that’s when shit got real. 24 hours before the procedure, I was instructed to drink the osmotic laxative polyethylene glycol (PEG) 3350, or “Miralax” or “Golytely.” PEG is also a common plastic coating, an industrial lubricant, and the base of many topical creams, so needless to say, it tastes… not good. I had to chug 2 liters in 90 minutes. 2 liters! That’s 6 red solo cups full to the beer line. Look at the size of the bottle in the first picture!! Then… after learning how much it tastes like plastic (because it is plastic), I had to chug 2 more liters the next morning.
Along with that, I took bisacodyl laxative pills. The result was that every hour or so I had to let out brown poop-water stuff. It’s expelled forcefully because your colon is accustomed to pushing out solid frictioned stools, which is odd but not terrible.
The “clear liquid” diet for the last 30 hours was the worst for me. My running-happy body has been happy running as a huge intake-output caloric system, but I had 180 calories of “Clear Ensure” to last an entire day. Our house is pretty cold too, so when I tried to study for the Step 1 board exam that afternoon, I was shivering. I attempted to hide under many covers and hibernate, but I woke up light-headed and dehydrated and hungry and still cold.
The next morning, I drank breakfast, then watched 007 Quantum of Solace while chugging laxative. James Bond be droppin’ bad guys while I be droppin’ liquid turds.
The Procedure
I can’t tell you a single thing about the procedure itself. My recollection is this: I was wearing a gown lying on my side in the dark endoscopy suite talking to the nurse and eating pizza in the car talking to my mom as she was driving us home. And my brain also has vague images of nearly falling out of the bed, a blue wheelchair, and standing up near a parking lot. Maybe.
Anterograde Amnesia
I was given two drugs: fentanyl and midazolam. Fentanyl is an opioid analgesic, like morphine and heroin but orders of magnitude more potent, which suggests to me that an endoscopy (getting a long probe snaked through your throat for 10 minutes) must be pretty distressing and/or painful. I wouldn’t know, because midazolam, a benzodiazepine, is a hypnotic that causes anterograde amnesia: the inability to form new memories.
And oh my goodness, anterograde amnesia is trippy.
When the procedure began, there’s a sharp edge in my memory where it just drops off a cliff. The bed was a papery firm-but-soft texture, and I was feeling chilly with the thin gown only hanging off my front. The suite was pretty spacious, and I had just noticed the two black scopes hanging from a pole. The nurse just gave me a nasal cannula and was saying something like “no, you really need to lie on your side!” And then…
They must have pushed the drug into the IV, because I remember nothing. Just… nothing!
The next pseudo-memory I have is of after the procedure, trying to leave, and nearly stumbling out of the hospital bed. I was adamant about walking myself, but nahhhh. I didn’t even get into the wheelchair on my own.
The wheelchair was blue and leathery. I think. Probably. Maybe.
I don’t know, because that “memory” of falling out of the bed is not a concrete memory. It’s more like a hazy impression. I know it happened conceptually, but I can’t remember who was there with me, what the room looked like, or even if I was dressed yet (though logically I must have been). Was my memory analogous to a slipping magnetic tape trying to take hold? Do I only remember the concept of falling because I was dwelling on the embarrassment, but only while I was under the influence? How did I get clothes on? And what happened before then?!?
I’m pretty sure I was able to hobble to the car after depositing the (blue leather (probably)) wheelchair in some sort of wheelchair receptacle (which in retrospect doesn’t make sense). I wonder if when I was struggling to form that memory, had I already dropped the previous one? I can’t remember if I remember!
Of course, we can hardly remember anything concretely from arbitrary days in the semi-remote past, but these are some fairly important details I failed to remember! In the car, right when my memory was finally taking hold, I found myself eating pizza and with with printed post-care instructions next to me. Some words were underlined, and I read them and was like “whoa, I was prescribed a PPI?” My mom responded “Yeah, you underlined that, and you were talking to the doctor about it.” Then I was like “Wait, I talked to the doctor? I don’t remember that at all… what drugs did they give me?” Mom: “I didn’t ask because you told me you already knew the medicines.” Me: “Wait. Dang it.”
First, I question the doctor’s decision to explain his findings verbally to an actively amnesic patient. It’s okay though; they wanted to be home for Christmas with family.
Second, I seriously didn’t remember what anesthetics they gave me. I remember the nurse said fentanyl, but only when studying benzos later did I deduce that the second drug was midazolam, probably.
Third, wow, I must have been comically annoying, asking the same questions over and over and over again.
Yup. My mom confirms this. When I first came to, I asked if I could eat now (no), had both procedures been performed (of course, why would they be separate?) and was there a chair for my mom (she was fine standing). Then through a couple cycles of drifting in and out of consciousness, I asked mostly three questions many times each: “How did I get here?” (wheeled on the bed) and “Did you see the pictures?” (no) and “Is the procedure done yet?” (yes). Then I collapsed on the bed again. Seconds later, slowly stirring “nyurggghhhhh … How did I get here? … Did you see the pictures? … Is the procedure done yet?” Repeat.
Honestly, I don’t remember asking any of those questions, not even once. Heck, two of the questions don’t even make logical sense sequentially!
Memory and Vulnerability
Anterograde amnesia is more than just a few lost hours. After all, every one of us humans loses 5-8 hours each day to non-memorizing sleep, also bookended by those drowsy moments when we’re drifting off or waking up.

This was a wholly new experience. I don’t think I’ve been sedated before; many people are sedated for the first time during wisdom teeth extractions, but I underwent that under aggressive local anesthesia. I also don’t drink much alcohol, so I haven’t woken up with the “what happened last night?” type of reaction. Quite frankly, I’ve always been frightened of that concept: blacking out from overdrinking alcohol. Not only do you have anterograde amnesia, you’re also uninhibited by copious amounts of alcohol and probably in a high-stakes social environment, so who knows…
Actually, no. I was about to write “who knows what happens then,” but then everyone there can pull out a phone and film the whole darned scene. Haha.
Midazolam + fentanyl is considered “conscious sedation” because apparently patients retain enough awareness to follow verbal commands. They probably instructed me to perform useful tasks like holding still or opening my mouth, but I wonder… if they told me to do ridiculous things, would I have done them? (I’m still dwelling on that hypothetical blacking-out-at-the-bar-with-your-buddies scene.) For this procedure, I’m sure that the medical team provided me a “safe place,” since they’re professionals who routinely care for patients in this half-conscious state, so I trust…
Well, hmmmm. I was about to write “so I trust nothing bad or funny or ridiculous happened,” but for goodness’ sake they stuck a camera up my butt!
less interesting addendum: Why I got a colonoscopy and endoscopy
The body treats iron carefully because it’s important for red blood cells and because bad bacteria use extra iron if it hangs around. It’s unexpected for me as a male to be iron deficient, because other than by bleeding copious amounts (say… every month?), my body has no dedicated pathway to lose iron even if it wanted to.
Thus, when a blood test in August showed my body’s iron stores had dropped precipitously over the last year, we had to investigate four broad etiologies: low intake (diet), bad absorption (GI health), bad incorporation (blood cell issues), or unexpected loss. It’d be pretty obvious if I were peeing red, coughing up red-tinted mucus, crying blood, or getting into routine knife fights, so the poop system is the most likely culprit for occult blood loss. To examine the GI tract, just take two cameras on long flexible tubes and have a look inside, starting from both ends.
We’ve investigated other causes. CBC otherwise normal. Thyroid hormones in normal range. Vitamin B12 levels fine. H. pylori antigen negative. No bleeding, phlebotomy, melena, GI discomfort. I think my diet’s balanced…? Since then, I’ve been using iron supplements and slight diet modification, and my values have rebounded to low normal ranges. I dunno what happened.
Update 1/29/16: He diagnosed me with GERD, or gastroesophageal reflux disease. My stomach is letting its corrosive fluid into the unprotected esophagus, which can bleed into my GI tract when damaged. More on this in a future post.