It’s the end of my radiology residency at Mount Sinai Hospital. I spent my final week reflecting upon my case log from residency, cases mined from four years of dictation, trolling the neuro list, and asking people for fun cases. That’s 1900+ cases of varying educational value, personal significance, or pure visual spectacle. Here are some highlights:
Case #1: a ureteral rupture, from my very first week of residency. I entered residency with intent, a programmable gaming mouse in hand, and knowing I wanted to build a case log for future teaching. I’m glad I followed through. 1900 cases is a lot!
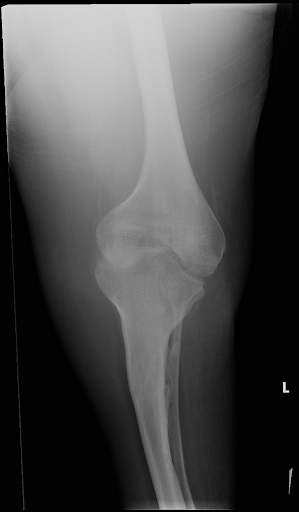
Case #33, Nail-Patella syndrome (Fong disease). I’m lucky to have encountered such a rare entity. Well, I also encountered and logged cases of Madelung deformity, melorheostosis, pyknodysostosis, ectrodactyly, polydactyly, and bracketed epiphysis, all in one month. How? Well, a willingness to try, a dedication to tabulation, and reckless speed. From the outset I specifically honed my mechanical and ergonomic efficiency, but admittedly that speed outstripped my nascent clinical acumen, and I was rightly criticized for being overconfident.

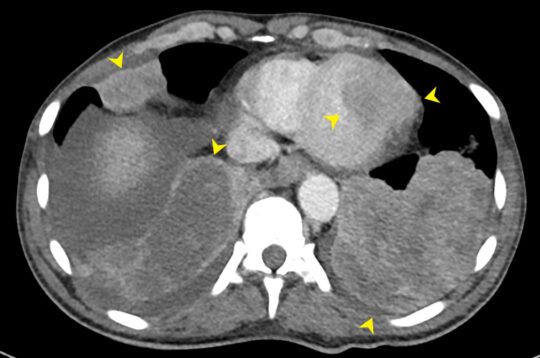
Case #152: “COVID,” from 4/3/2020. That’s when NYC went totally apocalyptic. Half of my department was deployed to the COVID units, but I stayed reading. Funny how I only logged three COVID cases; they transformed overnight from so novel to being publishable to being ubiquitous. At the peak, I changed my default chest x-ray template to COVID-positive…
Case #259, an ovarian dermoid cyst. It must’ve been a pretty attractive dermoid. It took some dedication to log this from my totally exhausting first week of nights. Thankfully, while COVID loomed for nearly the entire duration of my residency, its severity undulated, and case variety returned.
Case #483, a pituitary macroadenoma…?! A huge chunk of my logs are from just trolling (v. carefully and systematically searching an area for something) the neuro list. It’s a decent strategy for drilling search patterns, though not efficient for finding interesting pathology. Like, a pituitary adenoma?! Underwhelming.
Case #808, fetal aqueductal stenosis. Trolling exam codes with high pretest probabilities was actually high-yield. I saved a good number of fetal pathologies.
Case #1018, my AIRP case of wildly metastatic penile squamous cell carcinoma, which won runner-up most interesting GU case for my session (lol). Hilariously, this made me a temporary connoisseur of penile cases, and my colleagues would just forward more penile cases to me.
Case #266(ish), intracranial hemorrhage, missed by AI. Around March 2020, Sinai rolled out into clinical practice three artificial intelligence algorithms: intracranial hemorrhage, cervical fractures, and pulmonary emboli. I wasn’t impressed at first, exemplified by this case.
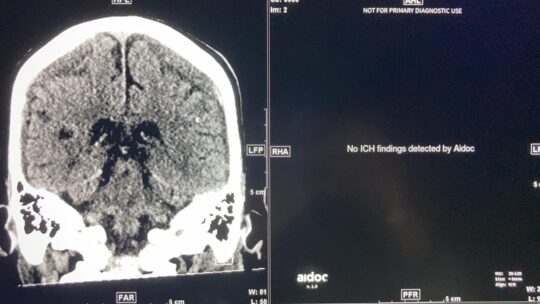
However, 3 years later, I completely trust our PE algorithm, altering my search pattern to rely on it. Check out Case #1894, an incidental lingual artery aneurysm. This is the future of radiology, and we are living it.
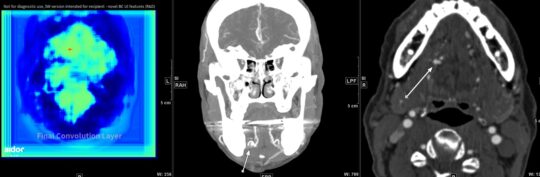
Having a leading AI vendor deployed here was a lonely bright spot in our frustrating, top-down, criminally underpowered and archaic rad IT landscape at Sinai. Take our quaint, quarter century-old GE PACS. Endearing, but inefficient. I also sorely missed Montage, a tool for searching the entire corpus of historical radiological reports, which would have been invaluable for mining teaching cases. This case log would have either been way bigger or way smaller…
Cases #226, #704, devastating myelomalacia from cervical trauma, notable because this was almost Katie and me. In August 2022, early in my chief year, we were nearly paralyzed and/or killed in a terrible car accident. Without exaggeration, that blasted accident completely derailed my chief year. Instead of spending extra energy on promoting the education role of chiefs. There’s a gaping void of cases from when the accident occurred.
Case #1464, HJ anastomosis dehiscence causing volvulus. This was my best prospective call: an entity I’d never seen presented, heard mentioned, or even thought possible. I’m proud, and also glad that the patient did all right afterwards.
Case #1928, giant ovarian mass, my final logged case. My final shift was covering the neuro fellow’s late shift, so I ended at 10 pm! My penultimate week mid-June was a late call week, which is even absurder; I was probably the only R4 on call in the entire country!!
Anyway, it’s weird saying a farewell to Sinai. My sense of radiology is inextricable from Sinai, and radiology is unimaginable in any other context. Can I still say “redemonstration?” Should I still associate a tortuous aorta with systemic arterial hypertension? What’s going to be the Yale equivalent of “macro attending”??

Four years it’s been. Just as long as high school, college, or med school, but these for years have been monumental. I felt more so a part of Sinai than any other place. This curious incubator has transformed me from a brash first-year to a beleaguered but decently skilled fourth-year chief. I hope I have contributed at least a little to improving Sinai Radiology.
To the attendings, coordinators, techs, nurses, fellows, and other residents who defined my time at Sinai: thank you too. Especially to Mark, Sanders, Rebecca, Cody, Darrell, Tim, Daryl, Kristina, and especially my co-chief Arthi. Thanks for being the best class ever.


To the junior residents: keep a case log!
